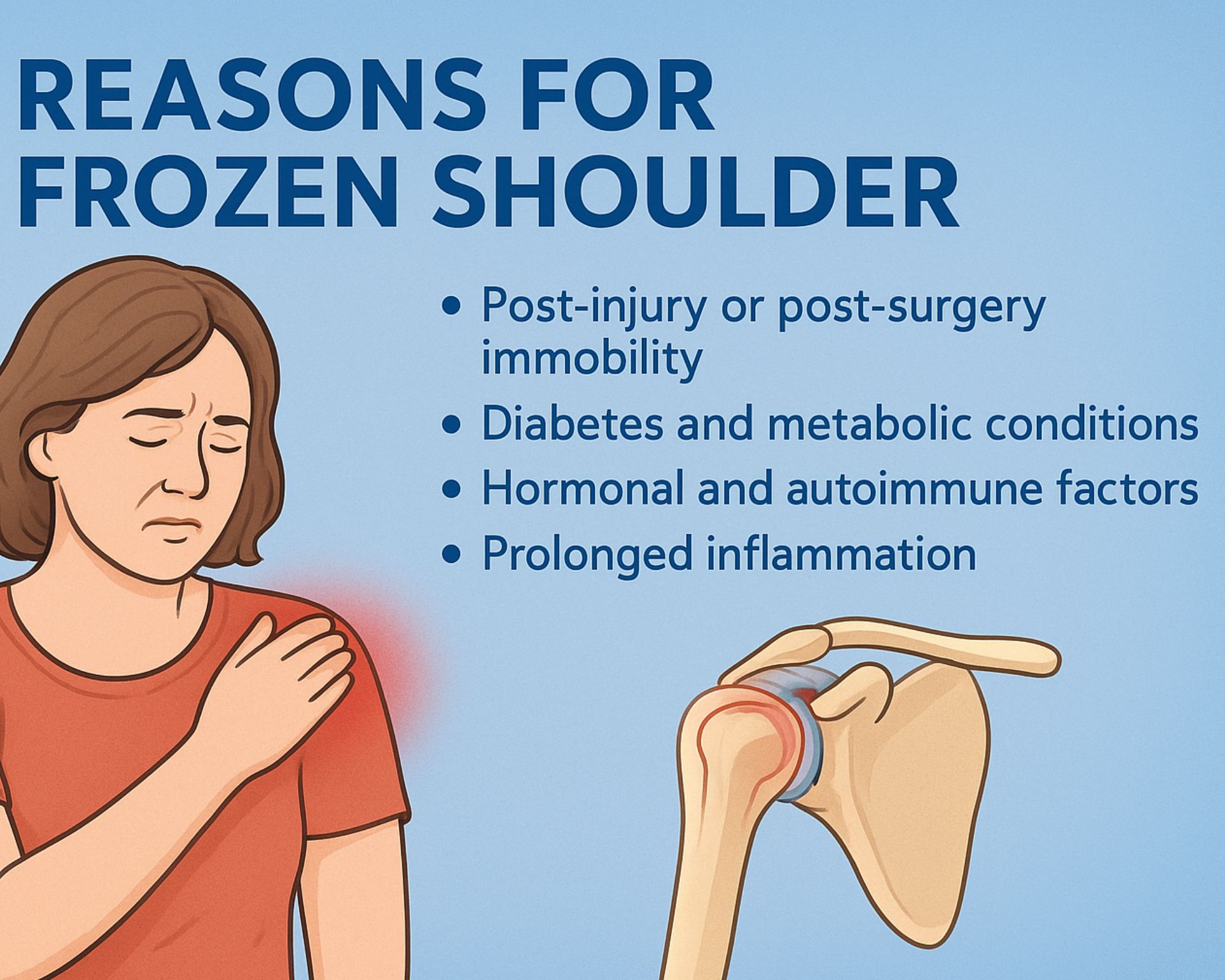
Why Frozen Shoulder Happens: Hidden Causes You Shouldn’t Ignore
Frozen shoulder, medically known as adhesive capsulitis, is a painful condition in which the shoulder becomes progressively stiff, restricting day-to-day movements like lifting the arm, wearing clothes, or reaching behind the back. Although the condition usually develops slowly, the reasons behind it are often a combination of underlying health factors, injuries, and age-related changes in the shoulder joint.
1. Post-Injury or Post-Surgery Immobility
One of the most common triggers for frozen shoulder is reduced movement after an injury or surgery. When a person keeps the shoulder still for too long due to pain or recovery—such as after a fracture, rotator cuff tear, or shoulder surgery—the capsule around the joint begins to tighten. Over time, this immobility leads to the formation of thick bands of tissue (adhesions), causing stiffness and pain.
2. Diabetes and Metabolic Conditions
People with Type 1 or Type 2 diabetes have a significantly higher risk of developing frozen shoulder. Although the exact reason remains unclear, high blood sugar levels are believed to make connective tissues thicker and less flexible. Other metabolic disorders like thyroid dysfunction, high cholesterol, and metabolic syndrome also increase susceptibility.
3. Hormonal and Autoimmune Factors
Hormonal fluctuations—especially in women between the ages of 40 and 60—may influence inflammation and connective tissue behavior. Some studies suggest that the immune system may mistakenly trigger an inflammatory response in the shoulder capsule, causing it to harden and shrink.
4. Prolonged Inflammation
Chronic inflammation inside the shoulder joint can gradually damage and stiffen the capsule. Conditions such as tendinitis, bursitis, or repetitive strain injuries often create an environment where inflammation persists, eventually progressing into adhesive capsulitis if mobility is restricted.
5. Age-Related Changes
Frozen shoulder is most often seen in individuals above the age of 40. With age, the connective tissues of the shoulder naturally lose elasticity. Even minor strains or periods of reduced movement can trigger a cycle of stiffness that develops into a frozen shoulder.
6. Neurological Conditions
People with neurological or mobility-limiting conditions such as Parkinson’s disease, stroke, or cervical spine issues often develop frozen shoulder. Limited arm movement, muscle imbalance, and changes in nerve function can contribute to tightening of the joint capsule.
7. Stress and Overuse Without Adequate Recovery
Although less commonly discussed, repetitive overuse without proper rest can irritate the shoulder structures. Over time, micro-injuries and continuous inflammation may lead to restricted movement. When the shoulder is kept still to avoid pain, the risk of freezing increases.
8. Idiopathic Causes
In some cases, frozen shoulder develops without a clear reason. This is known as idiopathic adhesive capsulitis. Even in such cases, subtle factors—like undetected micro-injury, stress-related inflammation, or mild metabolic imbalances—may be at play.
Conclusion
Frozen shoulder is rarely caused by a single factor. Instead, it is usually the result of reduced movement, underlying health conditions, and natural changes in joint tissues. Early recognition and regular mobility exercises play a crucial role in preventing worsening stiffness. With timely treatment—through physiotherapy, stretching, and controlled activity—most people gradually regain strength and flexibility in the shoulder.

